Positive ADEPT Phase 2/3 Results for Dupixent in Bullous Pemphigoid at AAD
Positive results from the pivotal ADEPT phase 2/3 study evaluating the investigational use of Dupixent (dupilumab) in adults with moderate-to-severe bullous pemphigoid (BP) were shared in a late-breaking oral presentation at the 2025 American Academy of Dermatology (AAD) Annual Meeting. BP is a chronic, debilitating, and relapsing skin disease with underlying type 2 inflammation and characterized by intense itch and blisters, reddening of the skin, and painful lesions.
Victoria Werth, MD, chief of the division of dermatology at the Philadelphia Veterans Administration Hospital, Professor of Dermatology and Medicine at the Hospital of the University of Pennsylvania and the Veteran's Administration Medical Center, and principal investigator of the study “People with bullous pemphigoid live with unrelenting itch, blisters, and painful lesions that can be debilitating and make it difficult to function daily. Moreover, current treatment options can be challenging for this primarily elderly patient population because they work by suppressing their immune system. By targeting the underlying type 2 inflammation, which is a key driver for bullous pemphigoid, Dupixent is the first investigational biologic to show sustained disease remission and reduce disease severity and itch compared to placebo in a clinical study.”
The ADEPT study met all primary and key secondary endpoints, enrolling 106 adults with moderate-to-severe BP who were randomized to receive Dupixent 300 mg (n=53) every two weeks after an initial loading dose or placebo (n=53) added to standard-of-care oral corticosteroids (OCS). During treatment, all patients underwent a protocol-defined OCS tapering regimen if control of disease activity was maintained. Sustained disease remission was defined as complete clinical remission with completion of OCS taper by week 16 without relapse and no rescue therapy use during the 36-week treatment period.
As presented at AAD, results for Dupixent-treated patients at 36 weeks, compared to those treated with placebo, were as follows:
20% experienced sustained disease remission, the primary endpoint, compared to 4% (p=0.0114)
40% achieved =90% reduction in disease severity compared to 10% (p=0.0003)
40% achieved clinically meaningful itch reduction compared to 11% (p=0.0006)
1678 mg reduction in cumulative OCS exposure (p=0.0220) on average and a 54% lower risk of rescue medication use (p=0.0016)
In this elderly population, overall rates of adverse events (AEs) were 96% (n=51) for Dupixent and 96% (n=51) for placebo. AEs more commonly observed with Dupixent compared to placebo in at least 3 patients included peripheral edema (n=8 vs. n=5), arthralgia (n=5 vs. n=3), back pain (n=4 vs. n=2), blurred vision (n=4 vs. n=0), hypertension (n=4 vs. n=3), asthma (n=4 vs. n=1), conjunctivitis (n=4 vs. n=0), constipation (n=4 vs. n=1), upper respiratory tract infection (n=3 vs. n=1), limb injury (n=3 vs. n=2), and insomnia (n=3 vs. n=2). There were no AEs leading to death in the Dupixent group and 2 AEs leading to death in the placebo group.
In February, the US Food and Drug Administration (FDA) accepted for priority review the supplemental biologics license application for Dupixent to treat BP. The FDA decision is expected by June 20, 2025. Dupixent was previously granted orphan drug designation by the FDA for BP, which applies to investigational medicines intended for the treatment of rare diseases that affect fewer than 200,000 people in the US. Additional applications are also under review around the world, including in the EU.
The safety and efficacy of Dupixent in BP are currently under clinical investigation and have not been evaluated by any regulatory authority.
BP is a chronic, debilitating, and relapsing skin disease with underlying type 2 inflammation that typically occurs in an elderly population. It is characterized by intense itch and blisters, reddening of the skin, and painful lesions. The blisters and rash can form over much of the body and cause the skin to bleed and crust, resulting in patients being more prone to infection and affecting their daily functioning. Approximately 27,000 adults in the US live with BP that is uncontrolled by systemic corticosteroids.
ADEPT is a randomized, phase 2/3, double-blind, placebo-controlled study evaluating the efficacy and safety of Dupixent in 106 adults with moderate-to-severe BP for a 52-week treatment period. After randomization, patients received Dupixent or placebo every two weeks, with OCS treatment. During treatment, OCS taper was initiated after patients experienced two weeks of sustained control of disease activity. OCS tapering could start between four to six weeks after randomization and was continued as long as disease control was maintained, with the intent of completion by 16 weeks. After OCS tapering, patients were only treated with Dupixent or placebo for at least 20 weeks, unless rescue treatment was required.
The primary endpoint evaluated the proportion of patients achieving sustained disease remission at 36 weeks. Sustained disease remission was defined as complete clinical remission with completion of OCS taper by 16 weeks without relapse and no rescue therapy use during the 36-week treatment period. Relapse was defined as appearance of =3 new lesions a month or =1 large lesion or urticarial plaque (>10 cm in diameter) that did not heal within a week. Rescue therapy could include treatment with high-potency topical corticosteroids, OCS (including increase of OCS dose during the taper or re-initiation of OCS after completion of the OCS taper), systemic non-steroidal immunosuppressive medications, or immunomodulating biologics.
Select secondary endpoints evaluated at 36 weeks included:
• Proportion of patients achieving =90% reduction in Bullous Pemphigoid Disease Area Index (scale: 0-360)
• Proportion of patients with =4-point reduction in Peak Pruritus Numerical Rating Scale (scale 0-10) score
• Total cumulative OCS dose
• Time to first use of rescue medication
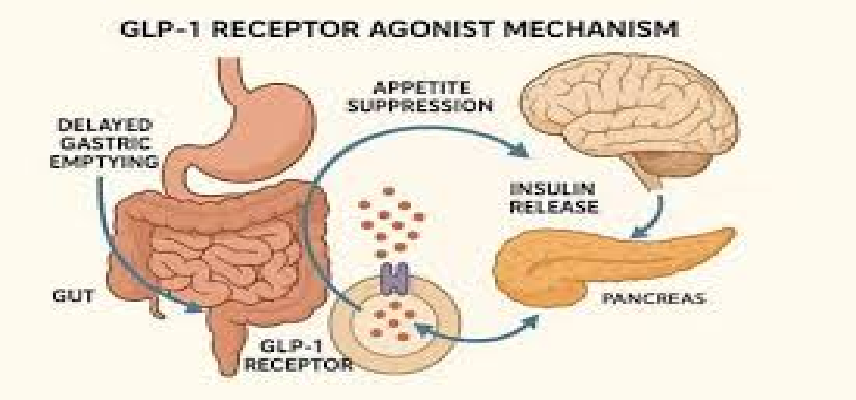
Dupixent (dupilumab) is a fully human monoclonal antibody that inhibits the signaling of the interleukin-4 (IL4) and interleukin-13 (IL13) pathways and is not an immunosuppressant. The Dupixent development program has shown significant clinical benefit and a decrease in type 2 inflammation in phase 3 studies, establishing that IL4 and IL13 are two of the key and central drivers of the type 2 inflammation that plays a major role in multiple related and often co-morbid diseases.
Dupixent has received regulatory approvals in more than 60 countries in one or more indications including certain patients with atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps, eosinophilic esophagitis, prurigo nodularis, chronic spontaneous urticaria, and chronic obstructive pulmonary disease in different age populations. More than one million patients are being treated with Dupixent globally.
Dupilumab is being jointly developed by Sanofi and Regeneron under a global collaboration agreement. To date, dupilumab has been studied across more than 60 clinical studies involving more than 10,000 patients with various chronic diseases driven in part by type 2 inflammation.
In addition to the currently approved indications, Sanofi and Regeneron are studying dupilumab in a broad range of diseases driven by type 2 inflammation or other allergic processes in phase 3 studies, including chronic pruritus of unknown origin, bullous pemphigoid, and lichen simplex chronicus. These potential uses of dupilumab are currently under clinical investigation, and the safety and efficacy in these conditions have not been fully evaluated by any regulatory authority.
Regeneron is a leading biotechnology company that invents, develops and commercializes life-transforming medicines for people with serious diseases. Founded and led by physician-scientists, our unique ability to repeatedly and consistently translate science into medicine has led to numerous approved treatments and product candidates in development, most of which were homegrown in our laboratories.

Optimize Your trial insights with Clival Database.
Are you exhausted from the uncertainty of trial insights pricing? Clival Database ensures the clarity in the midst of the global scenario for clinical trials to you.Clival Database is one of the best databases that offers an outstanding number of clinical trial data in terms of 50,000+ molecules and from primary regulatory markets as well as new entrants like Indian and Chinese markets.
With Clival, you get accurate positioning of historical sales data, patent database, company profiling, safety & efficacy, and prediction of launch of new innovative molecules helping you to align your research and driving down the cost.
To add value, we further break down our analytics for you so that improving your operational effectiveness; optimizing your clinical trials; and offering you accurate and high-quality data at lowest possible prices becomes possible.
Elevate your trial success rate with the cutting-edge insights from Clival database.
Check it out today and make more informed sourcing decisions! Learn More!